‘Cure diabetes’: Australia on verge of breakthrough
Australian researchers are poised to become the first in the world to take pancreatic islet cells from genetically modified pigs and transplant them into human patients. Their goal: To cure type 1 diabetes.
The culmination of decades of work was supported by multiple National Health and Medical Research Council grants and Breakthrough T1D grants.
They include an NHMRC Ideas Grant of almost $4 million to the University of Sydney transplantation professor Dr Wayne Hawthorne, last year.
“We’re now trying to get to the point where we can transplant these islet cells into patients” Hawthorne said.
“We’ve got animals surviving out past two years post-transplant, with no hyperacute rejection, no rejection, and with cured diabetes in that pre-clinical model.
“We’re hopeful, certainly by the end of our NHMRC grant, I would hope even sooner, that we would love to go to the clinic for very, very, very select patients.”
Pancreatic islets are clusters of cells within the pancreas. They secrete insulin, the hormone that plays a crucial role in regulating blood sugar levels. In people with type 1 diabetes, the immune system attacks and destroys these cells.
More than 140,000 Australians have type 1 diabetes.
They must supplement their body’s lack of insulin with daily injections to ensure their blood-sugar levels don’t get too high (hyperglycaemia). They also measure their BSLs multiple times a day to ensure they don’t fall too low, which is life-threatening.
Left untreated, diabetes can lead to short-term, life-threatening complications such as diabetic ketoacidosis and even death. In the long term, persistent high blood sugar can damage blood vessels, leading to nerve, eye, kidney, and heart problems.
You might like
On the other end of the scale, when a patient’s blood sugar levels get too low (hypoglycaemia), they must consume glucose. A “hypo” is usually accompanied by symptoms such as trembling, light-headedness, sweating, or irritability, which can alert a diabetic that they need to eat.
But Hawthorne said some patients could not tell when their blood sugar was low.
“If you can’t detect low blood sugar, you can’t give yourself food or even understand that you’re going to collapse into a coma and die. So, a number of these patients will sadly die,” he said.

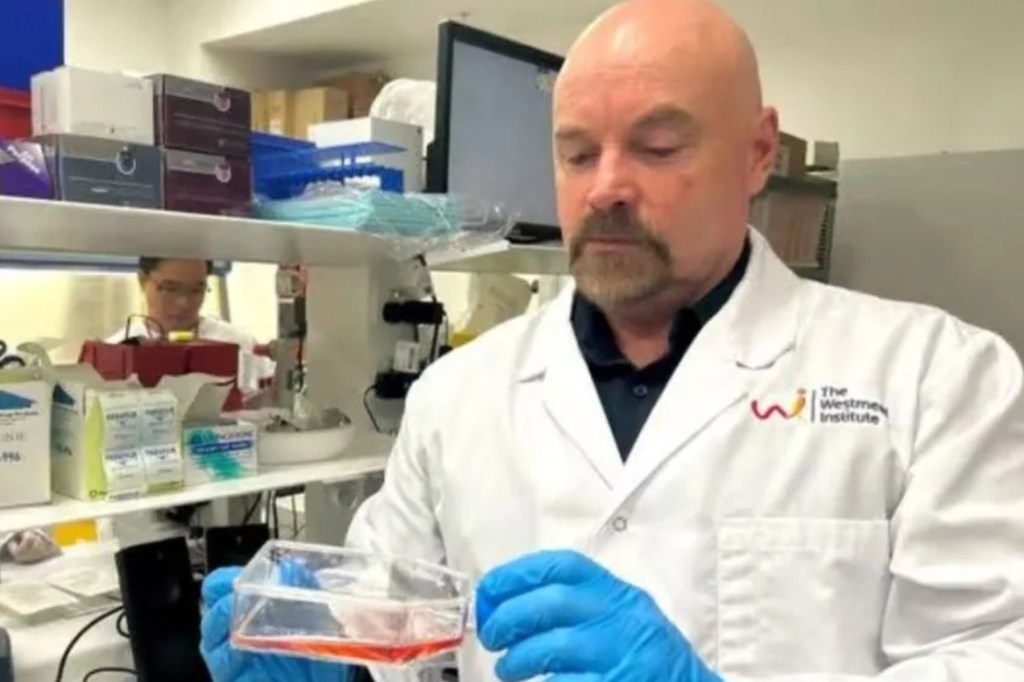
Human islets (red) sourced from a cadaveric human pancreas donor. Photo: Wayne Hawthorne
Hawthorne is director of the National Pancreas and Islet Transplant Laboratories at Westmead Institute for Medical Research and Westmead Hospital in Sydney. His team has performed decades of “allotransplants” – human-to-human transplants – to treat the most unwell diabetics.
The Westmead team developed combined pancreas and kidney transplants in the early 2000s to treat those patients who, due to poor luck in the genetic lottery, develop secondary complications of type 1 diabetes, including kidney failure.
“If we can put a pancreas in, we can prevent them subsequently going blind, getting nerve damage, kidney failure or losing limbs,” Hawthorne said.
The pancreas is a large organ with lots of blood vessels. Transplants involve major surgery that takes hours and has many potential complications. Doing so in combination with a kidney adds to the procedure’s complexity.
Additionally, not every donated pancreas is ideal. Age, excess fat, underlying comorbidity, including vascular disease, can rule out a whole organ transplant.
Once, these suboptimal organs were destined for the bin. Until, Hawthorne said, about 30 years ago, “we thought, why can’t we take that pancreas and try and extract the islet cells?”.
“We’ve developed a technology where we can basically put the pancreas in a blender and pull out the islet cells … It’s a very complex procedure that takes me eight-10 hours, but at the end of it, we have these beautiful separated islet cells,” he said.
Pancreatic islet transplants are a less invasive alternative to whole organ transplants, so can suit some type 1 diabetics with severe hypoglycaemia unawareness. The cells are infused into the patient’s liver where, soon after, they start to release insulin.
This restores the biofeedback mechanism that allows patients to prevent low blood sugar. It can even eliminate the need for daily insulin injections.
But, in practice, the pancreases donated by brain-dead patients aren’t always large enough for this procedure.
Stay informed, daily
“It’s only about 40 per cent of the time that we get enough islet cells to transplant into a type 1 diabetic patient,” Hawthorne said.
The organ must provide a minimum number of islets to justify giving the patient immunosuppressive drugs. These stop their immune system from rejecting the foreign cells but can also potentially make them more likely to develop infections and cancer.
This has led to a yawning gap between donor pancreas supply and demand, meaning patients wait years for a transplant or die before one arrives.
“My specialty has always been treating patients with type 1 diabetes by whatever means we can … that has meant allotransplants, and now we’re looking at xenotransplants,” Hawthorne said.
Xenotransplantation – taking cells, tissues or organs from one species and putting them into another – has been pursued by clinicians and scientists since the 1960s as a solution to the global organ shortage crisis. This year, the first clinical trials to transplant gene-edited pig kidneys into humans with end-stage renal failure will begin in the US.
The pigs are genetically modified to prevent the human immune system from recognising their cells as extremely foreign. But the GM pig lines cannot be imported into Australia due to our strict biosecurity laws.

Hawthorne and colleague isolate human islets. Photo: Wayne Hawthorne
Hawthorne and his co-collaborators – St Vincent’s Hospital Melbourne immunology chief Professor Peter Cowan, and Associate Professor Mark Nottle, who heads the reproductive biotechnology group at the University of Adelaide – have had to develop their own special pig lines.
“We have our own transgenic pigs, completely separate to the US and Europe and China and so on, and we’ve done the hard yards for decades to get us to the point now where we can use these for transplants,” Hawthorne said.
The cells of these pigs have been optimised to prevent hyperacute rejection, immune rejection, coagulation, and to provide additional immunosuppressive protection.
“I can potentially transplant these into a patient and give the minimum amount of immunosuppression, which means it’s more applicable to a wider range of patients,” he said.
“It will be a very select cohort of patients who, like our other islet transplant patients, suffer severe hypoglycaemia unawareness. We’ll treat very, very select patients first.
“The beauty of this, though, is we can potentially expand it to more patients than can currently receive islets from human donors.”
This won’t be possible without developing infrastructure for the procedure, including a specialised piggery to source the transgenic pig islet cells. Hawthorne said that required millions of dollars in funding.
“We will need to increase our… capacity to screen the product to transplant,” he said.
“We need to increase the number of associated teams of people to do the transplants, to do the observations of the patients, to continue following those patients, and then putting them in the [organ registrty] to ensure that we’re following those patients for development of potential problems.
“The question remains, are we going to get all the money from the health budget to do this, over someone dying of cancer or other diseases? There is only so much money in the bucket in the health system.”
This article first appeared in Cosmos. Read the original here








